The Importance of Foot Care for Diabetics
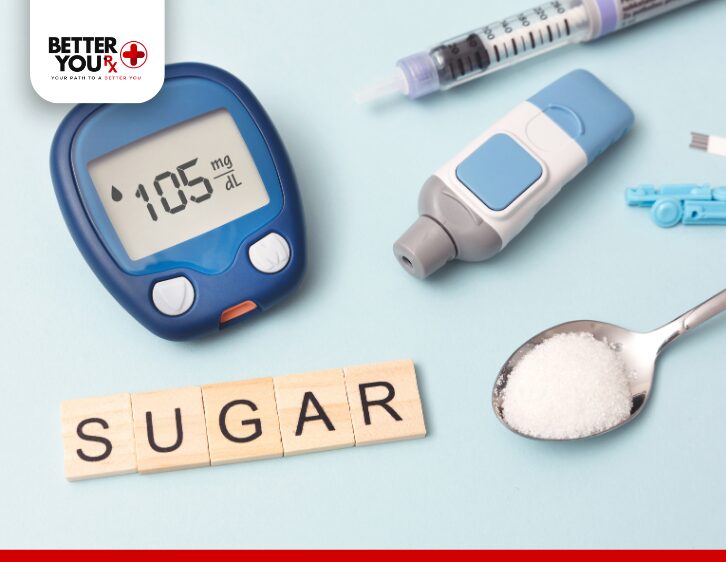
Diabetes is a chronic condition that affects various parts of the body, including the feet. People with diabetes are at a higher risk for foot problems due to nerve damage (neuropathy), poor circulation, and increased susceptibility to infections. This can lead to serious complications if left untreated, including amputations. Fortunately, with proper foot care, many of these issues can be prevented or managed. A comprehensive foot care routine is essential for anyone with diabetes, and it’s vital to understand the best practices for keeping your feet healthy.
Why is Foot Care Important?
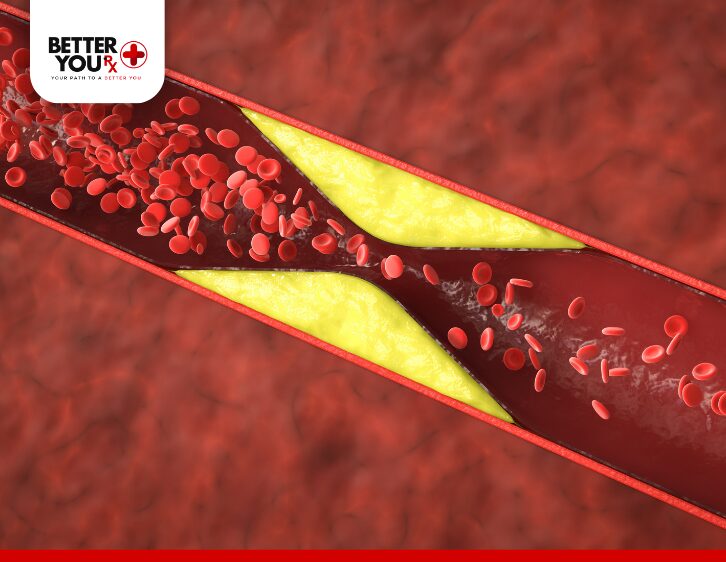
Diabetes can cause nerve damage and poor circulation, both of which can significantly impact the health of your feet. The nerve damage may result in a reduced ability to feel pain, heat, or cold, meaning cuts, blisters, or sores may go unnoticed until they become infected. Poor circulation also makes it difficult for your body to heal injuries, and it can lead to complications such as gangrene if an infection becomes severe.
By carefully monitoring and maintaining foot health, diabetics can reduce the risk of serious complications. Regular foot care, monitoring blood sugar levels, maintaining a healthy lifestyle, and seeking timely medical attention are all essential steps to avoid the more severe consequences of foot issues in diabetes.
Daily Foot Care: A Vital Habit

Daily foot care is the foundation of preventing foot problems in diabetics. Small habits that take just a few minutes a day can make a significant difference in foot health.
Inspecting Your Feet
It’s essential to inspect your feet daily, looking for any abnormalities like cuts, blisters, redness, swelling, or bruising. For those with poor vision, using a mirror or asking a family member or friend for assistance is a good alternative. Pay special attention to areas between your toes, as these are common spots for infections to develop. If you notice any changes, such as cuts or blisters, contact your healthcare provider immediately.
Washing Your Feet
Washing your feet daily in warm water and mild soap helps remove dirt and bacteria. However, diabetics need to be cautious with water temperature, as nerve damage can prevent you from feeling if the water is too hot. Always check the temperature with your fingers or elbow before submerging your feet in the water. Harsh soaps or hot water can irritate the skin, so use a mild, unscented soap to clean your feet.
After washing, it’s important to dry your feet thoroughly, especially between the toes. Moisture can contribute to fungal infections, and fungal growth thrives in warm, moist areas. Pat your feet dry with a soft towel, being careful not to rub too vigorously, as this can damage the skin.
Moisturizing Dry Skin
Diabetics may experience dry or cracked skin on their feet due to poor circulation. To prevent this, apply a moisturizing lotion or cream to the tops and bottoms of your feet. Be sure to avoid moisturizing between your toes, as excess moisture in these areas can lead to fungal infections. Choose a gentle, fragrance-free moisturizer to avoid irritating the skin.
Healthy Foot Habits: Key to Prevention
Developing healthy foot habits is essential to maintaining foot health and preventing injuries. Here are some habits you can incorporate into your daily routine to reduce the risk of foot complications.
Avoid Using Harsh Chemicals or Heat
Never use harsh antiseptics, heating pads, or hot water bottles on your feet without your doctor’s approval. These items can cause damage to the skin and increase the risk of burns or injury. Instead, stick to gentle methods for caring for your feet and consult with your healthcare provider about safe practices.
Protect Your Feet from Injury
Walking barefoot, even indoors, should be avoided at all costs. This includes walking on hard surfaces like tile or hardwood floors, as it exposes your feet to potential injury. Always wear shoes to protect your feet from cuts, bruises, and other injuries. Be cautious in environments where your feet may be exposed to hot or cold surfaces, such as hot sand or icy pavement.
Maintain Proper Posture and Circulation
Diabetics should be mindful of their posture and circulation. Avoid sitting with your legs crossed for extended periods, as this can restrict blood flow. Similarly, standing for long periods without moving can lead to poor circulation and discomfort. Make sure to get up and move around regularly to encourage blood flow and reduce pressure on your feet.
Toenail Care: A Crucial Aspect of Foot Health
Proper toenail care is an often-overlooked but important part of foot care for diabetics. If done incorrectly, toenail trimming can lead to injuries or ingrown toenails, which can become infected and lead to more severe problems.
How to Trim Toenails Safely
Trim your toenails after washing your feet, when the nails are softer and easier to cut. Cut the nails straight across to avoid ingrown toenails, and never cut into the corners of the nails. Be careful not to trim the nails too short, as this can lead to painful conditions. If you have difficulty seeing or reaching your toenails, it’s best to visit a podiatrist for help.
For individuals with thickened, yellowed, or damaged toenails, it’s essential to consult a healthcare professional for proper care. Never attempt to treat toenail conditions on your own, as improper treatment can lead to infections or further damage.
Footwear: Choosing the Right Shoes
Footwear plays a critical role in foot health, particularly for diabetics who have nerve damage or poor circulation. Wearing proper shoes can help protect your feet from injury and reduce the risk of sores or ulcers.
Choosing the Right Shoes
When selecting shoes, make sure they fit properly, provide ample space in the toe box, and offer support for your arches. Avoid shoes that are too tight, as they can cause pressure points and lead to sores or blisters. High heels, flip-flops, and pointed-toe shoes should be avoided, as they can increase the risk of injury.
It’s also important to choose shoes made of breathable materials such as leather, canvas, or suede. These materials allow air to circulate around your feet and help prevent moisture buildup, which can lead to infections. Inspect the inside of your shoes daily to ensure there are no rough spots or debris that could cause damage to your feet.
Special Footwear for Diabetics

If you experience chronic foot problems or have a history of foot ulcers or sores, ask your doctor about special diabetic shoes. These shoes are crafted to relieve pressure on key areas of the feet, enhance comfort, and offer extra support. Special insoles may also be recommended to help distribute pressure evenly across your feet.
Recognizing Signs and Symptoms of Foot Problems

Recognizing early signs of foot issues is crucial, as prompt attention can help prevent serious complications.Some signs to watch for include:
- Burning, tingling, or numbness in your feet
- Loss of sensation to touch, heat, or cold
- Changes in the color or shape of your feet or toenails
- Swelling, redness, or warmth in the feet or legs
- Painful or swollen areas, especially after prolonged standing or walking
- Infected or non-healing sores, ulcers, or blisters
If you notice any of these symptoms, it’s important to contact your healthcare provider immediately. Delaying medical treatment can result in serious complications, including infection, gangrene, or even amputation.
Potential Complications of Poor Foot Care
If foot problems go untreated, they can quickly become serious. Nerve damage and poor circulation from diabetes can slow healing and allow infections to progress quickly. Sores or ulcers that are not addressed may become infected, leading to complications such as gangrene. In severe cases, amputation may be necessary to prevent the spread of infection to other parts of the body.
To avoid these complications, it’s essential to maintain a daily foot care routine, monitor your blood sugar levels, and seek medical attention at the first sign of a problem.
Visiting the Doctor: Regular Check-Ups
Regular visits to your doctor are vital for monitoring the health of your feet. Your doctor should check your feet during every visit, with a comprehensive foot exam at least once a year. If you have a history of foot problems, more frequent exams may be necessary.
Your doctor can provide guidance on the proper care for your feet and recommend treatment options if issues arise. They may refer you to a podiatrist, a specialist in foot care, if necessary. If you experience persistent foot problems, such as sores or infections, seek medical attention promptly to prevent further complications.
Conclusion
Proper foot care is essential for people with diabetes to avoid serious complications. By adopting a daily foot care routine, choosing the right footwear, and staying vigilant for early signs of problems, diabetics can significantly reduce the risk of severe foot issues. Regular check-ups with your healthcare provider and prompt attention to any changes in your feet are crucial for maintaining good foot health. With the right care, you can keep your feet healthy and avoid complications that could affect your quality of life.